How to Talk to Injured Athletes
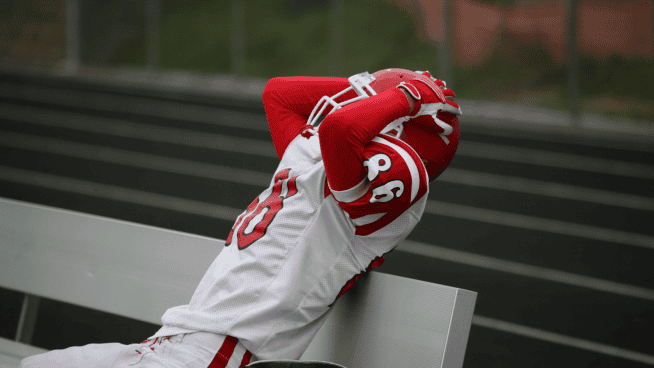
It’s every athlete’s worst nightmare.
The twist of an ankle, the buckling of a knee, or a pop within the shoulder can not only impact a player’s physical health, but can also wreak havoc on their mental psyche. Questions like, “Will I be able to play again?” or “Am I going to make it worse?” often race through their mind, creating an environment for worry, fear and uncertainty to flourish.
Although these questions are completely normal, sometimes it is other people’s word choices about an athlete’s injury that can significantly impact their road to recover.
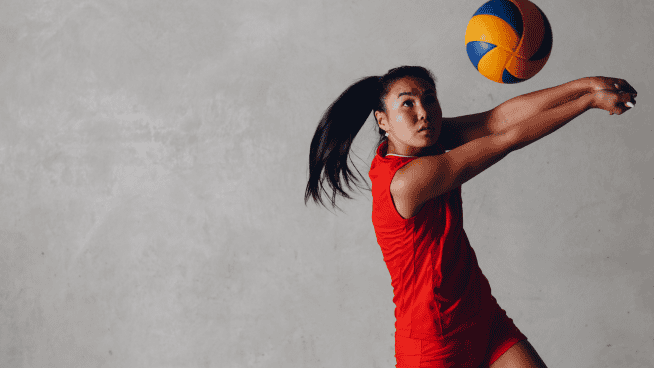
Take this situation for example. Susie Smith is a 16-year-old volleyball player who goes to her high school’s athletic trainer to get her knee evaluated. She points to her kneecap, says it hurts to squat and walk down stairs, and undergoes a thorough medical assessment.
All signs point toward patellofemoral pain syndrome, and the athletic trainer starts off by saying, “Well, your knee cap isn’t tracking right. You’re getting pain because the backside of the patella is grinding on your femur, which is what is causing your pain.” Insert face palm emoji now.
What’s wrong with this scenario? Several of the statements made by this hypothetical AT are what are known as “noceboes,” which essentially are words that can negatively impact a patient’s outcomes. For instance, the phrases “isn’t tracking right” and “grinding on your femur” have the capability of instilling fear into the patient’s mind, which as a result can reduce their willingness to exercise or participate in their sport.
As a physical therapist, I’ve heard colleagues and patients utilize the following statements:
- My pelvis is “unstable” and “out of alignment.”
- They said it is “bone-on-bone.”
- I was told to never lift over 10 pounds again.
- Bending that way will hurt your back.
- Squatting is bad for your knees.
- You have back pain because your core is weak.
Phrases like these make me cringe.
Yes, at times an individual’s back pain may be influenced by lumbopelvic strength, or squatting may be contraindicated following certain surgical procedures. But making blanket statements like these are often perceived as “end all, be all” by patients, especially following an injury. Why is this detrimental?
Ritter et al. saw that when patients with chronic low-back pain read pain-related words, there was greater activation of the part of the brain that senses pain compared to when they read less threatening words. But wait, there’s more! If we combine this with the fact that Swannell et al.’s research found that people perceived a heat laser stimulus as more painful after reading these similar painful words, just imagine what we have the potential to do to the psychological state of our athletes. Our words can add fuel to the fire and augment an athlete’s pain experience.
Not only can our words increase our athlete’s pain, but the fear induced by pathological language can increase stress. And why is stress bad?
Marucha et al. examined the effects of stress on wound healing. The researchers created punch biopsy wounds on the hard palate of the students during two different scenarios; one during summer vacation (couldn’t think of any better way to spend your summer), and the other three days before their first huge exam. The researchers then tracked to see how long it took each of the wounds to heal, and compared them between the two scenarios.
What did they find? The wounds that were made days before the big exam took nearly 40% longer to heal. Same type of wound, same person, all that changed were the situational stressors. Now why is that important? Think how stressed your athletes are if they are coping with an injury and can’t compete, and you keep reinforcing how weak they are, or how damaged their body is. The words we use may roll off the tip of our tongues, but those on the receiving end may have a hard time letting them go.
So what words can we say instead? The following list takes a look at common pathological word choices that can serve as noceboes for our athletes, and some alternative way to present the information:
This isn’t a complete list, but it provides a framework which may be more person-centered. Think about the words that you commonly utilize, and ask yourself how negative they are, or do they seem overtly threatening. Whoever said, “Sticks and stones may break my bones, but words will never hurt me” lied, and we have to think of the powerful impact our words can truly have on those around us.
Photo Credit: yacobchuk/iStock
References:
Ritter A, Franz M, Puta C, Dietrich C, Miltner WH, Weiss T. “Enhanced Brain Responses to Pain-Related Words in Chronic Back Pain Patients and Their Modulation by Current Pain.” Healthcare (Basel). 2016;4(3):54.
Swannell ER, Brown CA, Jones AK, Brown RJ. “Some Words Hurt More Than Others: Semantic Activation of Pain Concepts in Memory and Subsequent Experiences of Pain.” J Pain. 2016 Mar;17(3):336-49.
Marucha PT, Kiecolt-Glaser JK, Favagehi M. “Mucosal wound healing is impaired by examination stress.” Psychosom Med. 1998 May-Jun;60(3):362-5.
READ MORE:
- Applied Sports Psychology for Injury Recovery
- Trust the Process: 5 Things to Keep in Mind When Recovering From an Injury
- ‘What Can I Do?’ Is the Most Important Question You Can Ask After an Injury
RECOMMENDED FOR YOU
MOST POPULAR
How to Talk to Injured Athletes
It’s every athlete’s worst nightmare.
The twist of an ankle, the buckling of a knee, or a pop within the shoulder can not only impact a player’s physical health, but can also wreak havoc on their mental psyche. Questions like, “Will I be able to play again?” or “Am I going to make it worse?” often race through their mind, creating an environment for worry, fear and uncertainty to flourish.
Although these questions are completely normal, sometimes it is other people’s word choices about an athlete’s injury that can significantly impact their road to recover.
Take this situation for example. Susie Smith is a 16-year-old volleyball player who goes to her high school’s athletic trainer to get her knee evaluated. She points to her kneecap, says it hurts to squat and walk down stairs, and undergoes a thorough medical assessment.
All signs point toward patellofemoral pain syndrome, and the athletic trainer starts off by saying, “Well, your knee cap isn’t tracking right. You’re getting pain because the backside of the patella is grinding on your femur, which is what is causing your pain.” Insert face palm emoji now.
What’s wrong with this scenario? Several of the statements made by this hypothetical AT are what are known as “noceboes,” which essentially are words that can negatively impact a patient’s outcomes. For instance, the phrases “isn’t tracking right” and “grinding on your femur” have the capability of instilling fear into the patient’s mind, which as a result can reduce their willingness to exercise or participate in their sport.
As a physical therapist, I’ve heard colleagues and patients utilize the following statements:
- My pelvis is “unstable” and “out of alignment.”
- They said it is “bone-on-bone.”
- I was told to never lift over 10 pounds again.
- Bending that way will hurt your back.
- Squatting is bad for your knees.
- You have back pain because your core is weak.
Phrases like these make me cringe.
Yes, at times an individual’s back pain may be influenced by lumbopelvic strength, or squatting may be contraindicated following certain surgical procedures. But making blanket statements like these are often perceived as “end all, be all” by patients, especially following an injury. Why is this detrimental?
Ritter et al. saw that when patients with chronic low-back pain read pain-related words, there was greater activation of the part of the brain that senses pain compared to when they read less threatening words. But wait, there’s more! If we combine this with the fact that Swannell et al.’s research found that people perceived a heat laser stimulus as more painful after reading these similar painful words, just imagine what we have the potential to do to the psychological state of our athletes. Our words can add fuel to the fire and augment an athlete’s pain experience.
Not only can our words increase our athlete’s pain, but the fear induced by pathological language can increase stress. And why is stress bad?
Marucha et al. examined the effects of stress on wound healing. The researchers created punch biopsy wounds on the hard palate of the students during two different scenarios; one during summer vacation (couldn’t think of any better way to spend your summer), and the other three days before their first huge exam. The researchers then tracked to see how long it took each of the wounds to heal, and compared them between the two scenarios.
What did they find? The wounds that were made days before the big exam took nearly 40% longer to heal. Same type of wound, same person, all that changed were the situational stressors. Now why is that important? Think how stressed your athletes are if they are coping with an injury and can’t compete, and you keep reinforcing how weak they are, or how damaged their body is. The words we use may roll off the tip of our tongues, but those on the receiving end may have a hard time letting them go.
So what words can we say instead? The following list takes a look at common pathological word choices that can serve as noceboes for our athletes, and some alternative way to present the information:
This isn’t a complete list, but it provides a framework which may be more person-centered. Think about the words that you commonly utilize, and ask yourself how negative they are, or do they seem overtly threatening. Whoever said, “Sticks and stones may break my bones, but words will never hurt me” lied, and we have to think of the powerful impact our words can truly have on those around us.
Photo Credit: yacobchuk/iStock
References:
Ritter A, Franz M, Puta C, Dietrich C, Miltner WH, Weiss T. “Enhanced Brain Responses to Pain-Related Words in Chronic Back Pain Patients and Their Modulation by Current Pain.” Healthcare (Basel). 2016;4(3):54.
Swannell ER, Brown CA, Jones AK, Brown RJ. “Some Words Hurt More Than Others: Semantic Activation of Pain Concepts in Memory and Subsequent Experiences of Pain.” J Pain. 2016 Mar;17(3):336-49.
Marucha PT, Kiecolt-Glaser JK, Favagehi M. “Mucosal wound healing is impaired by examination stress.” Psychosom Med. 1998 May-Jun;60(3):362-5.
READ MORE:
- Applied Sports Psychology for Injury Recovery
- Trust the Process: 5 Things to Keep in Mind When Recovering From an Injury
- ‘What Can I Do?’ Is the Most Important Question You Can Ask After an Injury